NOTE: The Department of Health has responded to questions about conditions in the Covid isolation unit at Settlers Hospital and this response is included below.
As cases in Makhanda rapidly climb, private doctors, concerned about Settlers Hospital’s capacity to manage cases, have pleaded with the Department of Health to do whatever it takes to make the former Netcare section of Settlers Hospital available for all public and private Covid-19 cases.
Their call comes amid claims that there is insufficient nursing care in the current isolation section, and doctors struggle to find beds for their patients in private hospitals in Port Elizabeth or East London.
Under the current system at Settlers Hospital, private doctors may not admit their Covid-19 patients. Instead, the patient must present at Casualty, where the hospital’s doctors will examine them and refer them or admit them to an isolation ward.
“You are treated as a person under investigation (PUI) a source told Grocott’s Mail. “From there, you are taken to the isolation ward, where you are locked in and left.”

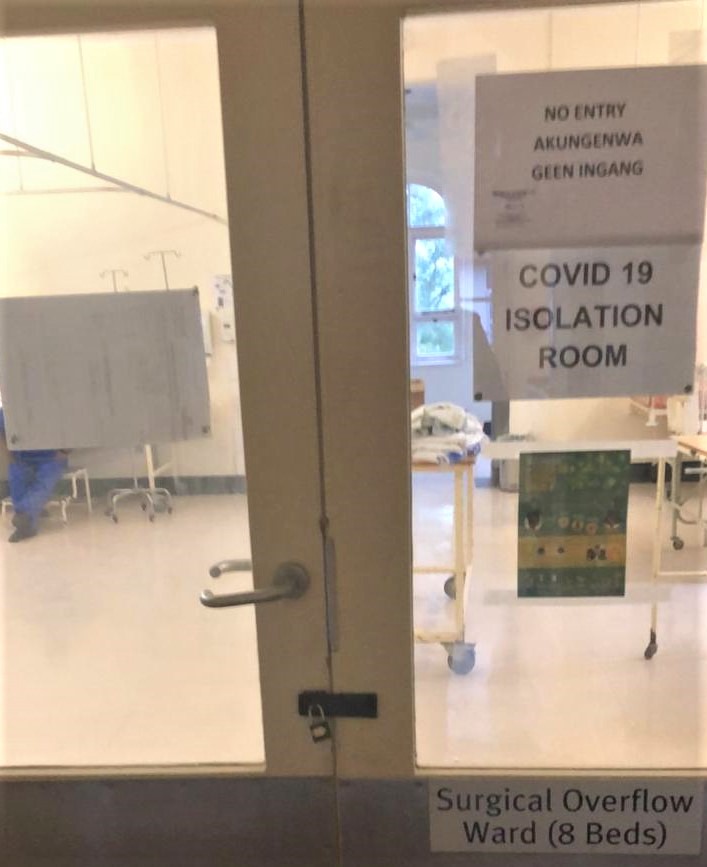
As seen in the accompanying photograph, the door to the isolation ward is padlocked from the outside.
“Once you are in there, your family is not allowed to visit you. You are locked up like a criminal.”
The conditions in there are bleak, the source said.
“There is very little comfort. There are no pillows. You can go for hours without anyone coming to check up on you.”


Protocol means that currently, during their time in a public hospital such as Settlers, a patient is no longer under the care of their own doctor. While private doctors respect the competence of their public health colleagues, they are concerned that their resources are too stretched.
In some cases, they believe, fear of the virus means nursing staff avoid the isolation unit, resulting in possible compromised care for the patients there.
“These patients require full-time nursing care,” said one doctor. “Those on an intravenous drip – that drip needs to be checked regularly.
“Current treatment for Covid-19 patients with respiratory distress is continuous high-flow oxygen through a nasal cannula or mask. That’s specialised machinery that needs continuous monitoring by someone who’s been trained to do so. It’s extremely important to monitor that a patient keeps their mask on, particularly older patients who may become confused.
“And it’s crucial that their oxygen saturation levels are very closely monitored.”
The doctor said even basic care (regular meals, cleaning the facility) was unreliable, let alone the specialised full-time nursing care required for COvid-19 patients.
As case numbers rise rapidly, doctors have pleaded with hospital management to do whatever it takes to get Netcare to allow the Department of Health to use the 32-bed former private section of the hospital as a dedicated Covid-19 section for both public and private patients.
“They should get people at low risk to work there – young people with no underlying illnesses,” said one doctor, who believes care for Covid-19 patients is compromised because health care workers are frightened.
“I would be happy to treat both public and my own private patients,” said a doctor. “This is a big community and we’re going to have a lot more cases.
“Bhisho hasn’t designated Settlers as a Covid treatment facility. They’re trying to pretend it’s not there. This is a big community and we’re going to have a lot more cases. We can’t just push it under the carpet.
“They must open that ward – just take the lock off the door.”
Netcare, which managed the private sections of the public-private partnerships at state hospitals Settlers and Port Alfred, closed their facilities there on 6 December. At the time, the Department of Health said there had been no formal agreement to terminate the relationship and that the matter of Netcare’s withdrawal had not been finalised.
The Department of Health had been in a public-private partnership with consortium Nalithemba at the two hospitals since 2009. Netcare is a 50% shareholder in Nalithemba and operates the private facilities at those hospitals. Settlers has 32 private beds (of 251) and Port Alfred 31 (of 60). These were the only private facilities operated by Nalithemba Hospitals.
This week, Grocott’s Mail asked Netcare whether they would consider allowing the Department of health to use the 32-bed facility at Settlers as a dedicated Covid-19 treatment facility.
Dr Chris Smith, consultant to the Nalithemba Board, replied as follows: “Netcare (Nalithemba Hospitals) are in discussions with the Eastern Cape Department of Health (EC DoH) regarding the final handover of the remainder of the project which would enable the EC DoH to optimise the utilisation of the facilities.”
READ: UNIONS BACK FRIGHTENED HOSPITAL WORKERS
DEPARTMENT OF HEALTH’S RESPONSE TO QUESTIONS FROM GROCOTT’S MAIL ABOUT SETTLERS HOSPITAL
Received from Department of Health at 6pm Friday 3 July
ALLEGED POOR NURSING CARE IN COVID 19 ISOLATION SECTIONS
- The isolation wards are allocated staff on a daily basis to care for the patients over 24 hours – both night and day duty. There is a unit doctor who is in the unit throughout the day.
- There is staff in each unit delegated by the supervisor to manage isolation units.
- There is a Unit Manager in each and every unit who monitors ward activities.
- There is an Area Manager who has oversight of each and every unit and manages challenges.
BELIEF THAT NURSES ARE AFRAID AND REFUSE TO WORK IN THAT SECTION
- No nurse has ever refused to take care of, or nurse, patients in isolation. Instead they are very keen, diligent, working beyond the call of duty.
- All hospital staff including nurses were trained to deal with Covid-19 patients and suspects
- There is an extended staff meeting every Tuesday, where a Covid update is given to staff and concerns addressed.
ALLEGATION THAT THE ISOLATION UNIT IS LEFT UNCLEANED AND IS DIRTY
- Cleaning services are outsourced to a private service provider and they always take care of the units.
- At some point, where the cleaners have to attend to other isolation wards after the discharge of a patient, there is a delay observed in cleaning. This is because most cleaners have to embark on deep cleaning of the unit to ready it for use by next patient.
- The Housekeeper has now delegated two cleaners to be responsible for isolation wards.
ALLEGATION THAT NURSES AND GENERAL WORKERS HAVE NOT BEEN PROVIDED WITH APPROPRIATE PPE
- No nurses nor general workers have ever said they have a problem with PPE.
- We have never had a problem with PPE as institution.
- The staff order PPE for each unit and keep it according to each unit’s needs.
- PPE Is controlled to ensure availability and reports are provided every Friday on the availability of PPE.
- The institution is receiving donations from Rhodes, Gift of the Givers etc. No shortages were ever noticed nor reported.
- Our staff always wear appropriate PPE according to their job requirements
- A Quality Assurance Committee, Health and Safety Committee and Unit Representatives monitor compliance with PPE.
- The PPE monitoring tool, based on stock level monitoring, indicates that staff are utilising PPE.
IRREGULAR MEALTIMES/ UNRELIABLE MEALS IN THE ISOLATION UNIT
- Catering is outsourced and served at regular times according to schedules by hostesses. The hostess hands over meals into the Isolation unit to a nurse wearing PPE.
ROOM PADLOCKED
- No padlocks are available or used in hospital wards.
- The doors are kept closed as a regulation of isolation wards.
TEN CONFIRMED COVID-19 PATIENTS
- To date [this response received 6pm Friday 3 July]10 confirmed Covid-19 patients Have been admitted to Settlers
- Five died in hospital due to Covid
- Seven died with Covid-related conditions
- Some are still awaiting results
- 1 recovered
- 2 are still admitted in the unit
Coping with Covid
Friday 10 July, 12-1pm
As case numbers grow in our town, so do the concerns of community members. In next Friday’s Forum we bring three expert panellists to provide guidance on how to manage Covid-19: what the numbers translate to in our everyday lives; how to manage a Covid case in your own home; and coping strategies from a psychologist. Plus two residents who have recovered from Covid-19 talk about their experiences of stigmatisation and support. This is a Zoom webinar that you can also watch live on Facebook or listen to later on RMR89/7. Please follow Grocott’s Mail’s Facebook page where we will post the registration details.
https://www.grocotts.co.za/2019/12/03/hospital-break-up-netcare-doh-must-explain/